Before you’re discharged from Swan Ward or the Bluebell Birth Centre you will be signposted to lots of information including our postnatal video which gives advice about the first few days and weeks after giving birth. If you choose to give birth at home, your midwife will let you know where to find these resources.
If you are not going home to your usual address following discharge from hospital, it’s important that you let us know.
Your postnatal care at home will be personalised and will depend on your needs and the needs of your baby however you can expect to be offered the following appointments.
Your baby’s birthday is day 0 so day 3 will be 3 days after baby is born.
Primary visit (midwife appointment on your first day at home)
Your midwife will visit you during the day, usually between 08:30 and 20:00, so we appreciate you staying at home during this time. If you have another appointment during your first day home, please let us know.
During your primary visit your midwife will offer to examine both you and your baby. Your midwife will offer to: feel your abdomen to ensure your uterus is shrinking back towards its original size, measure your blood pressure, and take your pulse and temperature. They will ask you questions about your recovery following birth, including blood loss and how you’re feeling physically and emotionally.
Your midwife will offer to examine your baby and if appropriate, weigh your baby. They will ask questions about your baby, including how many wet and dirty nappies your baby is having each day, and discuss feeding in more detail. Your midwife will check for any signs of jaundice (changes to skin colouring, often seen as yellowing of the face or body), and any signs of infection in the umbilical cord.
Your midwife will also discuss safe sleeping with you and ensure you’re aware of how to put your baby to sleep safely to reduce the risk of Sudden Infant Death Syndrome (SIDS).
Postnatal day 3
If you are breastfeeding or chestfeeding, you will be offered an appointment with a midwife or a support worker when your baby is 3 days old. This is to weigh your baby and offer feeding support if needed. This appointment will take place in your home or in our Postnatal Clinic in the Bluebell Birth Centre. Your midwife will let you know where your appointment will be held.
Postnatal day 5
Your baby will be reweighed when they are 5 days old. We will also offer the Neonatal Screening Test (NNST) otherwise known as a heel prick test. This involves your midwife collecting 4 spots of blood onto a special card. This is sent for screening of rare but serious conditions that, if treated early, can help a baby live a healthier life. This appointment will take place in your home or in our Postnatal Clinic in the Bluebell Birth Centre. Your midwife will let you know where your appointment will be held.
More information about this screening test can be found here. The information is available in other languages and in an easy read format.
Other visits
If there are any complications with your baby, such as a larger than normal weight loss on day 3 or 5, your midwife will put a plan into place which may involve more visits to monitor baby’s weight and may involve the infant feeding team to give you more support with feeding if needed. However, if you have any concerns about yourself or your baby following birth, you can call the Bluebell Birth Centre at any time for advice on 01926 495321 ext 6977.
Discharge from maternity services
If your baby has regained their birth weight and there are no concerns with either you or your baby, we would aim to discharge you from maternity services between 10 – 14 days. We will then hand over you and your baby’s care to the health visiting team. This discharge appointment may be face-to-face or over the phone, depending on circumstances.
Here at SWFT and across the country, we want to improve pelvic and perineal health throughout women and birthing people's maternity journeys. This is to reduce the number of women and birthing people living with pelvic health problems postnatally and later in life.
Your pelvis and perineum
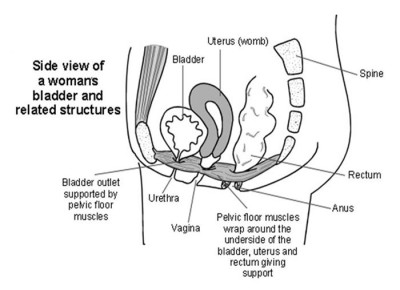
Your pelvis contains your bladder, uterus (womb) and rectum. These organs are held in place by the pelvic floor which is a set of muscles that forms a ‘hammock’ around them. Good muscle tone helps bladder and bowel control and prevents prolapse (when organs slip from their normal position and create a bulge in the vagina).
As your baby grows, the increased weight puts pressure on the pelvic floor. This can weaken the muscles and so it is important to build up strength through pelvic floor exercises.
Your perineum is the area between your vaginal opening and back passage (anus). It is made up of skin and muscles. Your perineum stretches as your baby’s head makes their way through the birth canal.
The pelvic health problems that can occur during pregnancy and birth
The pelvic and perineal health problems that can occur include:
- Perineal issues:
- Pain following perineal tears
- Perineal wound infection
- Bladder issues:
- Difficulties emptying the bladder
- Urinary incontinence (urine leakage)
- Bowel issues:
- Difficulties holding in wind (flatulence)
- Faecal incontinence
- Pelvic issues:
- Pelvic girdle pain (PGP)
- Pelvic organ prolapse
As well as the physical symptoms that the above can cause, they can also cause anxiety, depression, negative body image and sexual dysfunction so it is important to understand ways to optimise perinatal pelvic and perineal health.
Perineal tears
Approximately 9 in every 10 women who have their first vaginal birth will experience a type of perineal tear. This maybe a graze to the skin, or it could be tearing to the muscles, or an episiotomy (this is a cut through the vaginal wall and perineum).
There are 4 types of perineal tear which are graded according to severity:
- First degree tear: These affect only the skin. They usually heal well without any treatment.
- Second degree tear: These affect the skin and muscle of the perineum. They usually require stitches and heal well.
- Third and fourth degree tears: These are also known as obstetric anal sphincter injuries (OASI). They are complex tears which have extended into the anal sphincter. This type of tear affects approximately 3.2 women out of every 100 vaginal births.
- Episiotomy: This is a surgical cut made by a midwife or doctor to make more space for your baby to be born. They are not done routinely. An episiotomy may be recommended if you are having an instrumental birth, at risk of severe perineal trauma or if your baby’s heartrate drops and needs to be born quickly. If you have had an episiotomy you will need stitches to repair it.
How to reduce your risk of perineal tearing
Before birth
Perineal massage aims to increase the flexibility and elasticity of the perineal tissues. This may reduce your risk of severe tearing or the need for an episiotomy. It can be done from 35 weeks, ideally 3-4 times a week. You may choose to ask your partner to help with this. It is not advisable to do perineal massage if you have a vaginal infection, thrush or genital herpes.
The Royal College of Obstetricians and Gynaecologists (RCOG) has produced a perineal hub which contains lots of useful information including how to do perineal massage. My expert midwife also provides a guide on how to do perineal massage with some videos.
At the time of birth
Birth position: Try and adopt a birth position that is most comfortable for you. If you have an epidural, lying on your side can be helpful.
The NHS has produced a helpful video on what positions are best for giving birth.
Warm compress: Your midwife or doctor will offer to gently use a warm compress against your perineum as your baby’s head becomes visible.
Manual perineal protection: This is when your midwife or doctor uses their hands to support your perineum. This is done during the birth of your baby’s head and shoulders. It can be done in most positions apart from water or on a birthing stool.
Controlled birth: Your midwife or doctor will support you with breathing techniques to help control the birth of your baby allowing the perineum time to stretch slowly.
What happens if your perineum does tear during childbirth?
Approximately 9 in every 10 women who have their first vaginal birth will experience a type of perineal tear. For those who are having their second or subsequent vaginal birth the chances of tearing are reduced.
After birth, with your consent, your midwife or doctor will carefully examine your perineum, vagina and anus to see if you have a tear and if so what type. This can be uncomfortable and so if you do not have an epidural it may be helpful to use some entonox (gas and air) during this examination.
If you have grazes, a second-degree tear, or episiotomy this can usually be repaired in the room where you gave birth by the midwife. If you have sustained a third or fourth degree tear you will need to be taken to the operating theatre. Your repair will be carried out by a doctor and you will be given a spinal or epidural so that you have good pain relief.
Caring for your stitches
If you have stitches, they will generally dissolve between 2-4 weeks.
It is important to:
- Keep the area clean. Only use water to wash (you can return to using your usual products once the area has healed). Dab yourself dry with a clean flannel or towel.
- Change your sanitary pads regularly and wash your hands before and after you go to the toilet.
- Keep hydrated. Try and drink 2 litres of water a day. This supports recovery and also less concentrated urine stings less as it passes over the vulva and perineum.
- Eat a balanced diet. This will help keep your stools soft and avoid constipation.
- Maintain good toilet posture! When you are on the toilet, place your feet on a small footstool so that your knees are higher than your hips. This helps to straighten your bowels. Try to relax and don’t strain as this weakens your pelvic floor.
Your midwife will offer to look at your stitches. This is to check that you are healing well and that there are no signs of infection.
It is rare for stitches to come undone by themselves. However, stitches may breakdown if there is an infection, or pressure on the stitches from bleeding underneath. This can leave an open or gaping wound.
There is information on the RCOG perineal hub regarding what to do if you are concerned about perineal wound breakdown. The Pelvic Obstetric and Gynaecology Physiotherapy (POGP) provides some information about good bowel habits.
Pelvic floor exercises
Daily pelvic floor exercises can reduce your risk of incontinence both during pregnancy, after you have birthed your baby and later in life. You can do your pelvic floor exercises in any position, but initially it may be easier to do them lying down or sitting. Squeeze the muscles as if you are holding in wind. While you hold, tighten and lift the front muscles as if you are stopping yourself passing urine. It should feel like a squeeze and lift.
This video provides step-by-step instructions on how to do pelvic floor exercises.
You can buy the NHS Squeezy App (small one off payment) which comes with a pre-set exercise plan and the ability to set reminders.
In the early days, following birth, you may not be able to feel your muscles working, but don’t give up! Keep going and you will soon feel the muscles strengthening!
Pelvic girdle pain (PGP)
PGP is used to describe pain at the front and/or of the pelvis. It can also affect your hips and thighs. PGP can affect 1 in 5 pregnancies and is caused through the increased weight on your pelvis as your baby grows. If you are experiencing pain or ‘clicking’ in your pelvis, which is worse when you move then tell your midwife or doctor. They will refer you to the physiotherapist.
Pelvic, Obstetric and Gynaecological Physiotherapy (POGP), the Royal College of Obstetricians and Gynaecologists (RCOG), Tommys, the NHS all have lots of useful information about symptoms, diagnosis and treatment.
Pelvic organ prolapse
This occurs when the organs within the pelvis slip from their normal position. This is caused by weakening of the pelvic floor. There are different types of prolapse which depends on how far the organs have moved. It is experienced by approximately 1 in 10 women who are over 50 years of age. You may not have any symptoms, but may feel a bulge, and/or have bladder or bowel problems or feel uncomfortable during sex. It is diagnosed through an internal examination. Treatment options include pelvic floor exercises, lifestyle changes, pessaries or surgery.
The RCOG and POGP have lots of useful information about pelvic organ prolapse.
Sexual intercourse and contraception post birth
You and your partner may be anxious about having sex after you have had a baby, particularly if you have experienced a perineal tear. The appearance of your vulva may look different than it did before birth. This is a normal change, but if you have any concerns, ask your GP or midwife.
The decision to have sex should be based on when you both feel physically and mentally ready. Try talking to your partner and choosing a time when you both feel relaxed. Lubricating gel can be helpful. YES provides lots of information about lubricants and vaginal wellbeing.
It is possible to become pregnant again very soon after the birth of your baby, even if you are breastfeeding. You usually ovulate (release an egg) two weeks before period, so it is possible to get pregnant before your period. It is advisable to use condoms until you have spoken to your GP to discuss other methods of contraception.
The NHS website provides information about contraception after birth.
Resources and support
- RCOG Perineal tears hub. Developed by clinical specialists to provide information about how to reduce tears, treatment you may be given and how to help recovery.
- The MASIC Foundation. This is a charity which supports women who experienced severe perineal tearing. The charity is run by injured women and healthcare professionals who are committed to reduction of injury during childbirth. masic.org.uk
- Birth Tear Support (BTS).This is a Facebook Group offering peer support for women who sustain severe and complicated tears.
- Bladder and Bowel Foundation. A charity which provides support for people who are living with conditions that affect their bladder or bowel.
- Pelvic, Obstetric & Gynaecological Physiotherapy (POGP). A professional membership organisation that aims to provide evidence-informed care and advocacy.
- NHS Episiotomy and perineal tears. Information about the different types of tears and recovery.
Your health is important, both during pregnancy and afterwards. It is important to recognise that health encompasses more than just the physical and that mental wellbeing is equally significant. In fact, mental health issues are more common than physical health issues during pregnancy, impacting up to 20% of women and birthing people.
Here are some tips and steps you can take to help you to feel physically and emotionally at your best during pregnancy and after birth:
Diet
What you put in to your body is important. You can support your mental wellbeing by eating a healthy, balanced diet with regular meals. Also reducing alcohol intake (stopping is ideal) and stopping smoking will help you have a healthy pregnancy.
Sleep and rest
Your energy levels may fluctuate so it is important to make time to relax and try to get regular sleep. You might find mindfulness or meditation useful to assist with winding down and the below suggested apps can help:
Physical activity
If you are already doing regular physical activity then you do not need to stop. Talk to your midwife or doctor if you think you might be doing too much. If you would like to be more active, have a think about doing something that appeals to you, such as swimming, yoga or walking. All are excellent ways to keep fit, lift your mood and help you sleep.
Ask your midwife about local exercise classes.
Relationships
This is a time to think about who you have around you to share your pregnancy with. Think about who will be around to support you during your birth and after your baby arrives. Let your family and friends help you with routine tasks, such as shopping or housework.
Relationships can change during pregnancy. If you are concerned about this, please talk to your midwife or doctor.
Antenatal education
There is a lot to learn about what to expect in pregnancy, during birth and the postnatal period. Try to attend antenatal classes to learn about the changes to your body and how to prepare for a baby. This will help you feel more in control of what can be an exciting but challenging time and help you to meet others who are expecting babies around the same time as you.
Ask your midwife for further information.
Talk to someone
Pregnancy and the period after childbirth are significant times of change in a person’s life. It is common for women, birthing people and their partners to experience many different emotions during this time. It is often an exciting time, but you may also have mixed feelings about being pregnant. Many women and birthing people are worried about the impact that a baby will have on their lives and how they might cope with these changes. These worries might include:
- The changes in your role (becoming a parent, stopping work)
- The changes in your relationships
- Whether you will be a good parent
- Fear that there will be problems with the pregnancy or the baby
- Physical health problems and pregnancy complications
- Fear of childbirth
- Lack of support and being alone
All of these anxieties are common and can be normal. However, as many as 1 in 5 women will experience a mental health issue in pregnancy or after birth. If your anxieties are impacting your day-to-day life, speak to a health professional. Talking to other people and sharing your feelings can be helpful.
Please speak to a healthcare professional if you notice changes in your mood that are lasting much longer than is normal for you. There is plenty of support in the local area and you can self-refer to NHS Talking Therapies and Parents in Mind (catchment for women and birthing people with a CV postcode) using the links below:
Please tell your midwife, GP or obstetrician if you have an existing mental health problem or have had a mental illness in the past. They can make sure that you get the individualised care and support you need from a specialist perinatal mental health midwife and/or a perinatal mental health team.
Learn more about perinatal mental health services.
Pregnancy and post-birth wellbeing plan
Creating a wellbeing plan might help you to start the conversation with your partner, family, friends or midwife about how you are feeling and what might help you during pregnancy:
Further information
To find out more about your body after pregnancy and birth, and for advice about how to help your body recover, click on the following links:
We advise that you use contraception for at least 21 days after your baby is born. For information about sex and contraception after birth, click on the following links: